The power of data, analytics, and predictive modeling has the potential to significantly improve human health and address the affordability challenge in the United States.
Evernorth Health Services manages pharmacy benefits, specialty care, and care delivery for more than 100 million people across the country. Our position at the center of the health care system gives us important data and insights that we leverage to build solutions – while protecting patient privacy – to deliver better and more affordable care. This approach offers the promise of better health outcomes across the entire health care system.
To demonstrate the power of this analytical approach, Evernorth is making available new data and a new framework for analyzing health care cost drivers in America. Knowing the conditions and types of care that consume health care spending is fundamental to identifying and prioritizing opportunities to improve health. Beyond the aggregate data, we can further understand and address localized and patient-level challenges, consistent with state and federal privacy laws.
The new data can provide insights into many crucial questions. What conditions represent the most significant share of health spending in a particular community? What types of care (e.g., pharmacy, inpatient services) are driving spending related to a particular condition? What types of service have high variability in per-patient cost? Do particular providers or therapies represent a disproportionate share of costs? What is the utilization of low-value services that have poor clinical evidence? Are there proactive strategies that can be deployed to promote health and wellness?
This approach holds incredible potential for improving the entire system and offers lessons for America’s public programs. By thinking differently about data, state and federal health programs can be more efficient and responsive to health trends. By answering the right questions, we can find the right solutions to unlock better health and help solve the affordability challenge in America.
What’s Driving Health Spending?
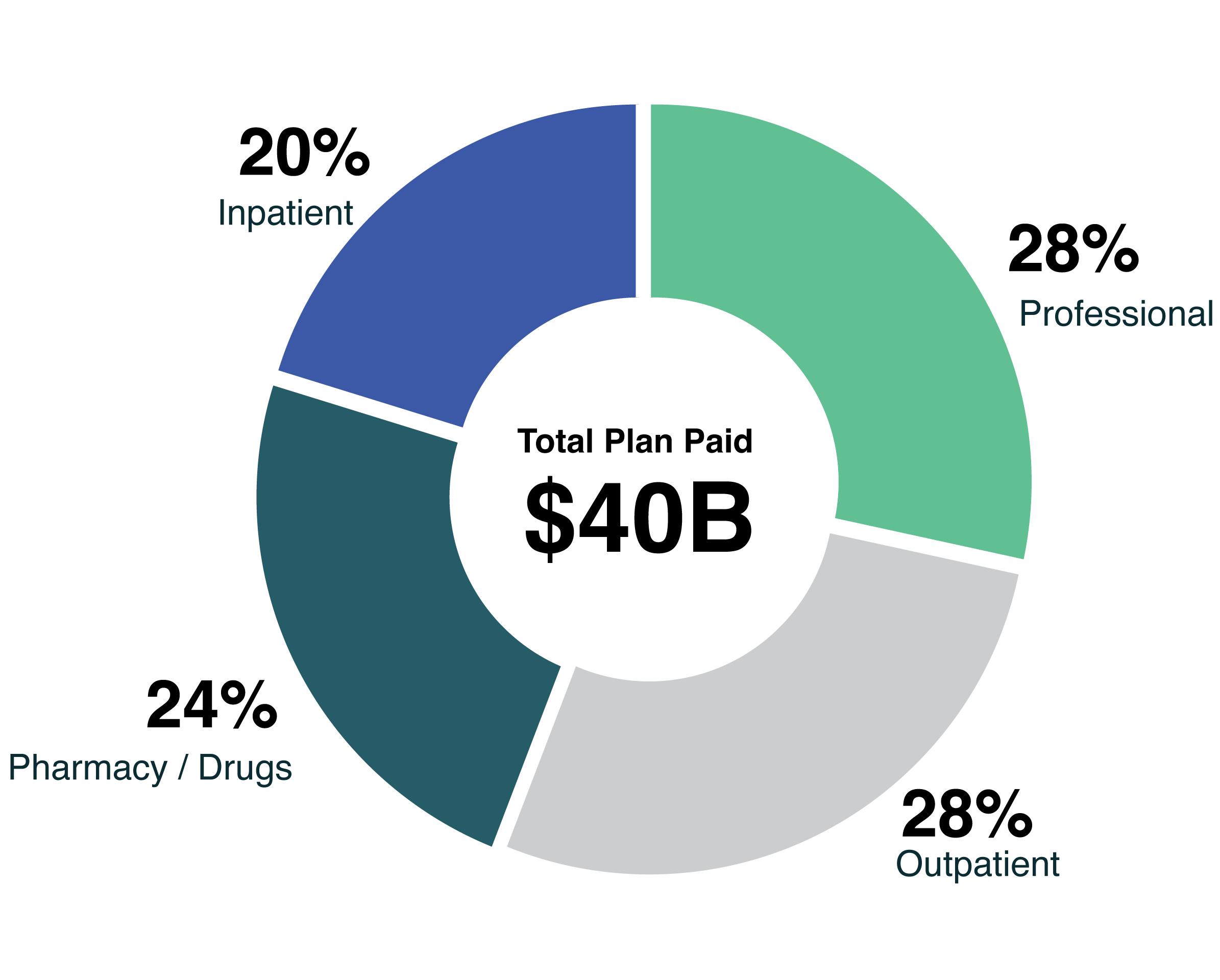
This chart, from the Evernorth Research Institute, shows total spending for a group of 7.2 million commercial customers (under 65 years old) with claims in 2021. Holistically, the chart shows how much was spent on various condition categories and the types of care that were used by this group of patients.
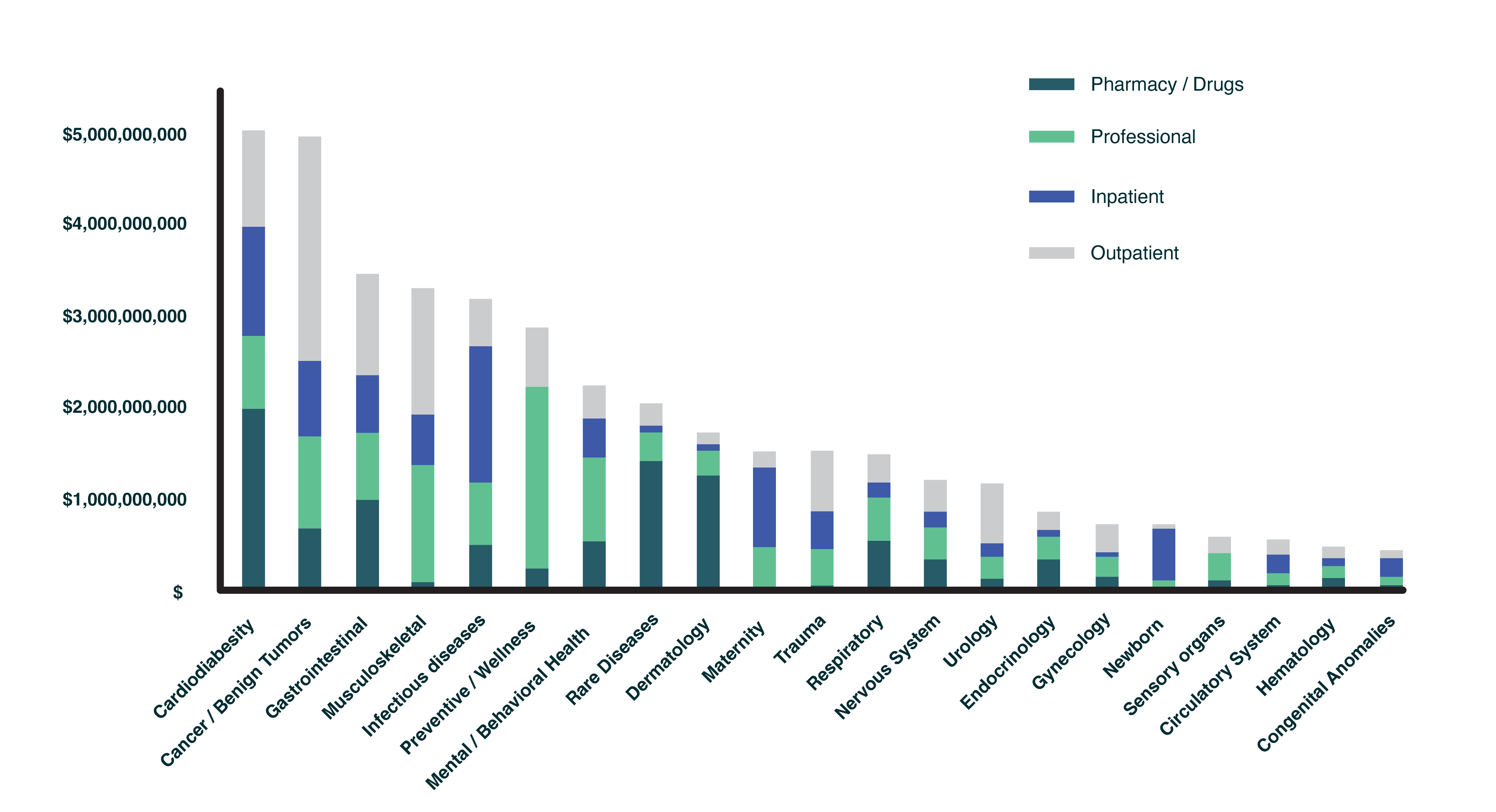
Data and experience indicate that we can better identify similarities and variances in services used when conditions with similar treatment pathways or sets of providers are examined together. For example, we know that cardiovascular health, diabetes, and obesity are all closely tied, so we look at them as a set of interconnected challenges. This group – cardiodiabesity – represented the largest share of spending in 2021. Treatment for tumors was a close second, followed by gastrointestinal conditions. Musculoskeletal conditions ranked fourth when we excluded musculoskeletal injuries and autoimmune musculoskeletal diseases.
We can further analyze the drivers of health care spend by exploring distribution of types of claims and top conditions within each category. Prescription medications filled using a pharmacy benefit accounted for 24% of spend across all conditions, but 39% for the cardiodiabesity category. Diabetes type 2, the top spend driver, was associated with 21% of the total cardiodiabesity category spend. Drugs filled through the pharmacy benefit accounted for 84% of diabetes type 2 spend. Year-over-year comparisons can identify additional useful trends in both health and care settings associated with treating a condition.
While this chart offers national data, Evernorth can create similar aggregate analyses for employers, health plans, labor unions, public programs, or other payers. Clients can look at their spending and health utilization trends to help inform future benefit design changes and improve affordability. We can also use data to help prevent future gaps in care and cost drivers by using predictive modeling to proactively anticipate a person’s needs to keep people healthier.
Turning Insights into Action
It is helpful to know what share of health spending can be attributed to particular conditions, but it is more powerful to understand why that is and what can be done about it. By digging deeper into the numbers, we can identify specific challenges and, more importantly, begin to solve them. This data enables Evernorth and our clients to identify strategies to control costs and help improve the health of their workforces.
For example, we may find that a particular health care provider or prescriber in a region is responsible for a significant cost spike. Then, we can work to bring down prices or drive patients to a more affordable setting of care. Or, data may reveal that important screenings are taking place at a lower rate than expected, and we can make sure that patients are not missing necessary preventive care.
Often, interventions are about promoting wellness to mitigate or prevent future health challenges. For example, one group of patients may benefit from a smoking cessation program, while another group with a high share of pre-diabetic patients could see improvements in their health with the use of health management tools. The following are two examples of how data can be put into action.
Data Driving Action
Breaking down barriers to health and wellness
The combination of Evernorth data and analytic capabilities allows for the identification of lower cancer screening rates in specific plans, geographies, and/or underserved communities. These advanced capabilities help identify challenges a population has to receiving the screenings. It could be as simple as lack of transportation or as complex as the lack of availability of health services. Our actionable intelligence helps us understand the challenge so we can find the right path forward to solve it. Through partnership and collaboration, Evernorth can make recommendations around education, support services, or specific solutions to help improve access to care and screening rates.
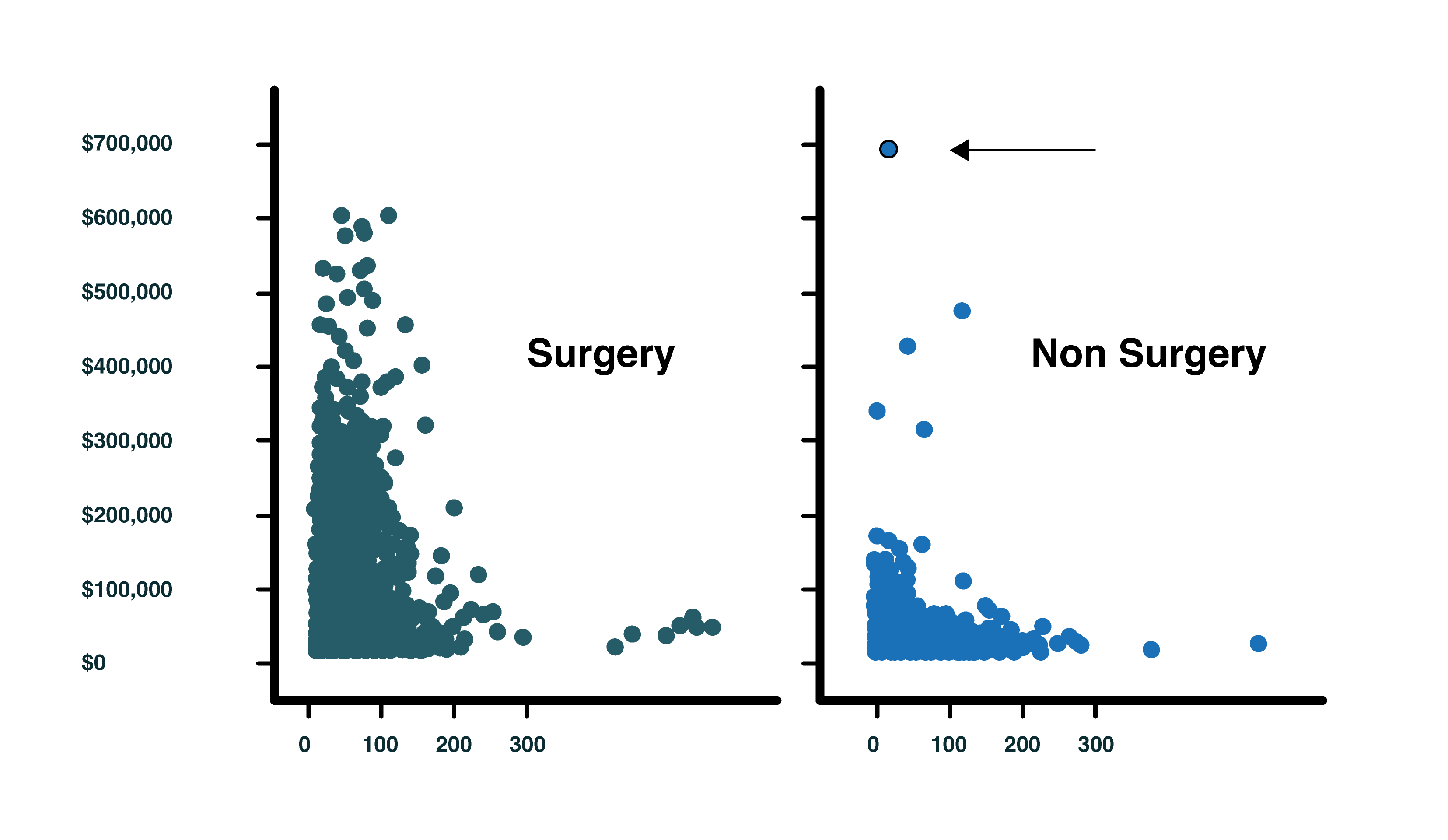
Identifying a cost outlier and finding a savings solution
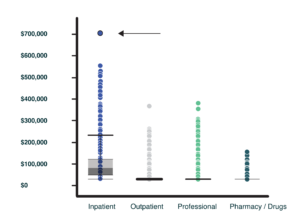
Data can tell a story. The story can be one of success through measured improvements in health outcomes or one of opportunity through the identification of a cost outlier. Evernorth tools have the power to enable exploration, identification, and research. The chart below shows an overview of treatments and costs incurred by patients with musculoskeletal conditions involving back pain. Using visual analytic techniques, outliers can easily be identified. The tools enable analysts to dig deeper and understand the drivers of the variation, which helps to determine the best way to mitigate the outliers if needed. In some cases, it may warrant the suggestion of managing the provider network in a different way. In other cases, the outcome may be suggestions for added care resources. The technology allows Evernorth to conduct analyses and make the right recommendation to help patients make informed decisions.
How Policymakers Can Think About This Data
Evernorth is leading a data-driven approach to care, using our capabilities to help solve the biggest challenges in health care. This research can serve as a model for making health care more personalized, efficient, and value-based. Public programs, for example, have the ability to use data to promote wellness and root out inefficiencies. Learnings like this that are developed in the private market can inform the approach taken by public programs such as state Medicaid programs or the Veterans Health Administration. Likewise, innovative pilot projects could be developed to implement similar care improvement and cost control initiatives across both public and private markets. Evernorth is committed to partnering with policymakers to share actionable intelligence and policy solutions while producing data insights that can spark change across the health care system.


